
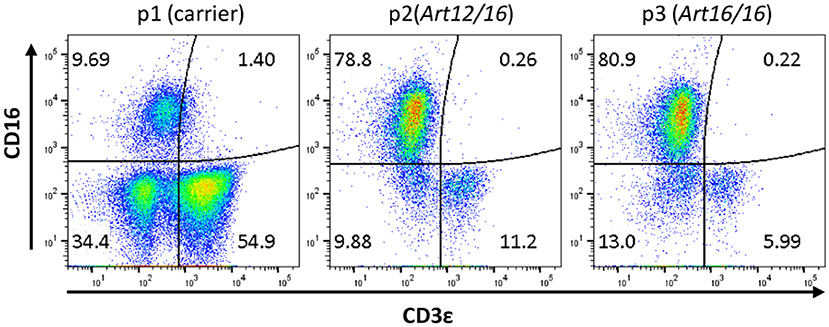
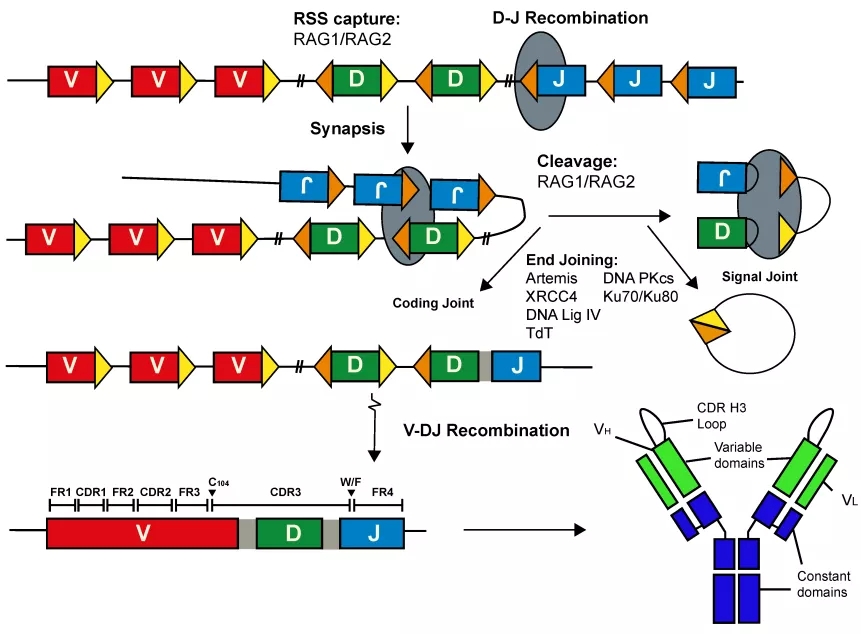
Numerous recently identified related defects allow T-cell development on the one hand but compromise T-cell function on the other by affecting proximal or distal steps in intracellular signaling. Interestingly, T cells may even be found in normal numbers in some SCID patients ( Roifman et al. All affected individuals, without exception, will have a fatal outcome unless the immune system is promptly restored by means of strict isolation and prophylactic antibiotics, followed by hematopoietic stem cell transplantation or, in some specific cases, gene therapy ( Dvorak et al. Regardless of the immunologic phenotype, patients with SCID share similar clinical features, including early-onset severe respiratory tract infections, severe infections with opportunistic pathogens, chronic diarrhea, and failure to thrive. SCID patients also display variable expressions of B and NK cells stemming from a specific genetic defect, and are therefore usually categorized into having either SCID with no T lymphocytes but with B lymphocytes (T − B + SCID) or SCID with neither T nor B lymphocytes (T − B − SCID) ( Al-Herz et al. As a result, the number of T cells, as determined by fluorescence activated cell sorting (FACS) analysis, is extremely reduced and cell function, as determined by response to mitogenic stimulations, is completely absent ( Cooper et al. A typical SCID patient is characterized by thymic dysplasia and arrest in T lymphocyte maturation (T − SCID phenotype).
Severe combined immunodeficiency (SCID) is the most severe form of inherited primary immunodeficiency.
Moreover, taking into consideration the milder clinical phenotype associated with transplacentally acquired maternal T cells in SCID patients, we believe that these cells may provide some degree of immunity and prevent autoimmunity, even though they do not actually function to protect against infections. We propose that coexistence of autologous and maternal T cells in patients exhibiting mild OS symptoms was rejected because it had not been studied before and not because the cells are mutually exclusive. This patient had both self-reactive cells and transplacentally acquired maternal T cells, allowing us to simultaneously evaluate the function and tolerance capacities of both cell types. An unusual case of an immunodeficient SCID patient with a mild OS phenotype is also presented. This review provides an updated functional characterization of transplacentally acquired maternal T cells and compares them with the T cells of an OS patient. The traditional view is that self-reactive cells and transplacentally acquired maternal T cells cannot occur concomitantly in the same OS patient. One distinctive feature of SCID patients, which can sometimes resemble the clinical picture of OS, is the presence of alloreactive cells that originated from transplacentally acquired maternal T lymphocytes. In some cases, however, T cells may be affected by defects that allow some T-cell development but compromise T-cell function such as in Omenn syndrome (OS), which is characterized by impaired T cell differentiation in the presence of abnormal self-reactive cells.
Patients with severe combined immunodeficiency (SCID) typically present with profoundly reduced T cells.


 0 kommentar(er)
0 kommentar(er)
